Home » News » 2025 » August
News Brief
Aug. 6, 2025 |
By: Caitlyn Miller
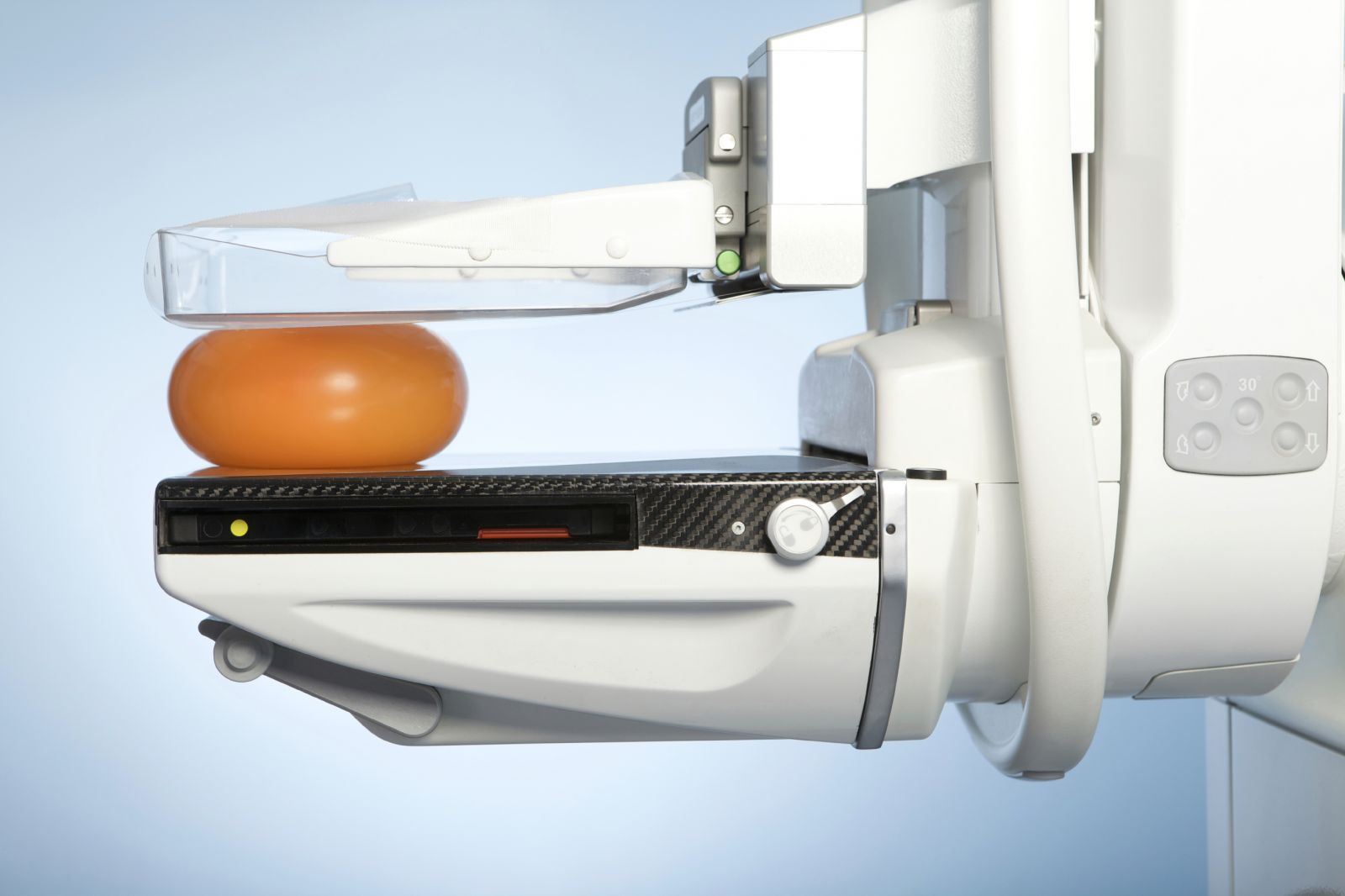
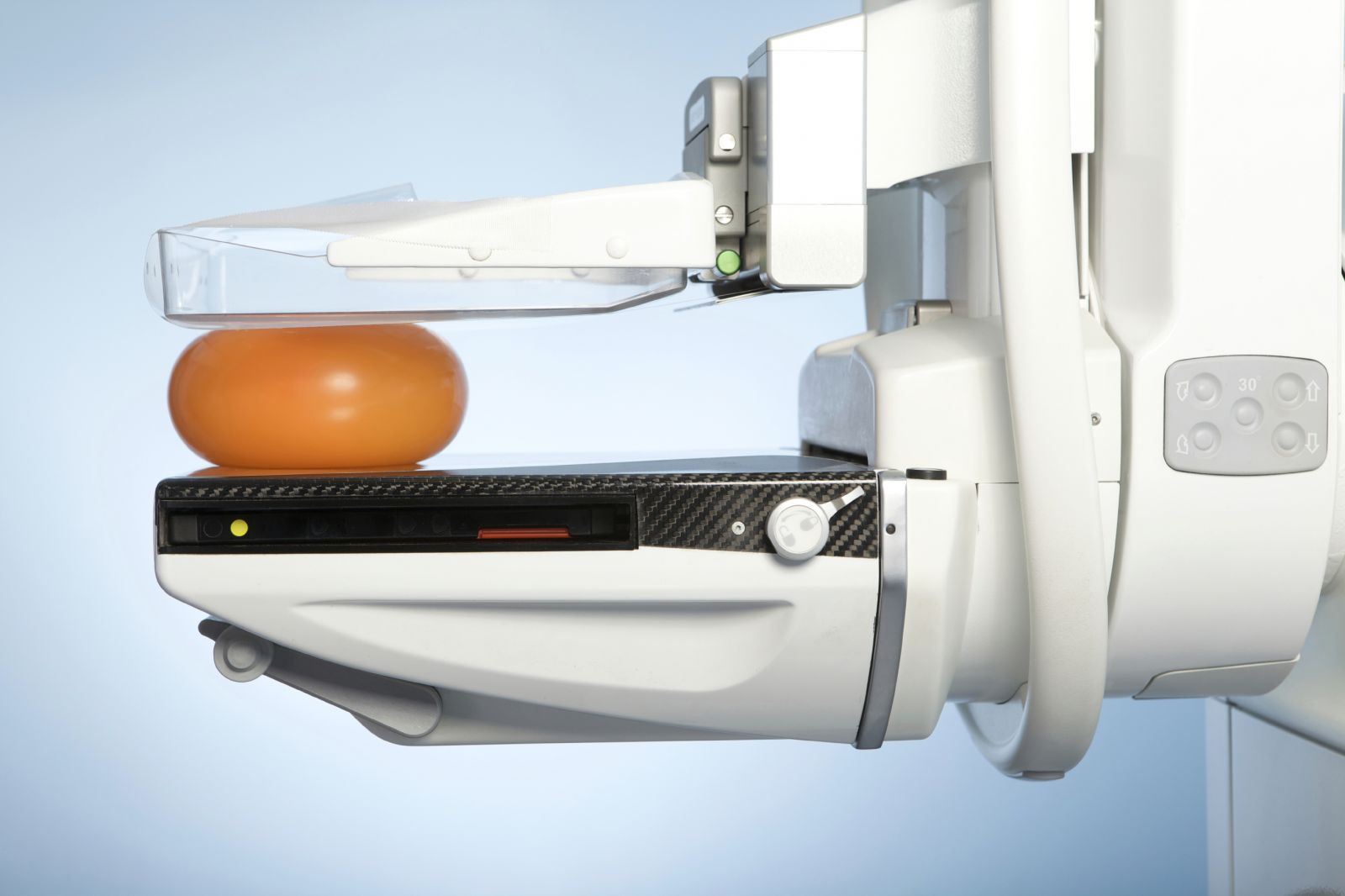
The impact of expanded mammography coverage in Missouri
© 2025 Harvard Health Publishing® of The President and Fellows of Harvard College
A newly released study highlights the impact of changes to Missouri state law that expanded insurance coverage for mammography screenings, revealing several notable trends.
-
Women on Medicaid in Missouri were 45% more likely to receive screening mammograms compared to those enrolled in Medicare Advantage (MA) plans.
-
Utilization of digital breast tomosynthesis (DBT), an advanced imaging technology, was 64% higher among Missouri Medicaid recipients than among similar populations in neighboring states that did not adopt the expanded coverage.
-
In general, Missouri women with Medicaid were about 9% more likely to undergo screening mammography than women in bordering states without the same coverage enhancements.
Lead author Dr. Amy K. Patel, medical director of the Liberty Hospital Breast Care Center in Kansas City, spoke about the findings in a video interview following the publication of the study in the Journal of the American College of Radiology.
“Essentially, our findings demonstrate if you provide coverage for screening, patients will get screened,” emphasized Dr. Patel.
Looking ahead, Dr. Patel mentioned the possibility of future research that would analyze long-term health outcomes and cost savings from early detection. She also indicated that follow-up studies could assess the effects of additional breast cancer screening legislation passed in Missouri in 2020 and 2023.
“For me, this is just part one of hopefully many analyzes coming down the pike that overall, hopefully demonstrate the benefits of insurance coverage for our patients, not just in the state of Missouri, but like I said, hopefully we can see similar findings in states across the United States,” added Dr. Patel, an associate professor of radiology at the University of Missouri-Kansas City.
![]()